Genomic technologies to reveal the correlations between Gut microbes and human health
The human intestine is a diverse and dynamic micro-ecosystem with a large number and variety of microorganisms, demonstrating a wide range of interactions with the host and also among each other. The normal intestinal flora plays a pivotal role in maintaining human health as a natural barrier. Changes in the internal and external environment of the body can also affect the structure of the intestinal flora, and once the intestinal flora is dysregulated, it may cause gastrointestinal or even systemic diseases. Therefore, the structure and function of intestinal flora have become a hot spot for research in life science and medicine. That is why the study of gut microbiota functionality holds substantial significance.
Gut microbiota complexity and host relationships
Genomic technologies such as amplicon sequencing, metagenomic sequencing, meta-transcriptomic sequencing, and metabolomics enable detailed investigations into the composition and activity of gut microbiota in humans and other animals. (1-5) The results provide deep insights into the rich diversity of gut microbiota, revealing a complex, interconnected community with crucial roles in host metabolism, physiology, and immunological functions. (1-6)
Sometimes the results of these technologies offer surprising new insights into host-microbiota relationships. (1, 4) For example, in a 2019 study, Tito et al. used 16S rRNA and 18S rRNA amplicon sequencing to examine the prevalence of Blastocystis (a single-cell eukaryote, SCE) in a Western population cohort. Although Blastocystis subtypes are often thought to be human parasites, this study suggested that Blastocystis is in fact, a common component of rich and diverse gut microbiota communities—that is, with healthy guts (30% prevalence in the non-clinical cohort versus 4% in the inflammatory bowel disease [IBD] cohort). (1) If we take another example into account, a 2021 study by Bi et al. used metagenomic, metatranscriptomic, and metabolomic analyses to identify the presence of a low-diversity, low-biomass prenatal gut microbiome in fetal lambs. Although it has been assumed that fetal gut colonization occurs during birth, this study suggests that colonization begins in utero and that the prenatal gut microbiome is metabolically active. (4) Studies such as these remind us how much we have yet to understand about the complexity of gut microbiota.
Dietary influences on gut microbiota composition and host health
Associations among gut microbiota composition, diet, and host health have been studied for decades. There is considerable evidence that dietary composition, such as the amount of fiber or grains consumed, can have short- and long-term effects on host health and nutrition. (2, 7) A 1984 study by Mitsouka reported age-related changes in the numbers of various gut bacteria species. Yet diet composition offsets those effects. Elderly men following a fiber-rich “mixed Japanese diet” experience less-drastic age-related changes in gut microbiota composition and a reduced incidence of hepatic carcinoma as compared to men consuming a “Western diet”. (7) More recently, a 2021 study by Xie et al. used 16S rRNA amplicon sequencing and shotgun metagenomic sequencing technology to examine the cecal microbiome composition of sheep gut feeding on a high grain (HG) diet. Their results showed that HG-diet-fed sheep experienced changes in cecal microbiome composition that persisted even after the end of the four-week HG diet. (2)
There is still so much to learn about the associations among gut microbiota composition, influences such as diet and medication, and the health effects in a human host. One complex example involves obesity and type 2 diabetes (T2D). There is growing evidence for the role of gut microbiota in obesity and T2D, but the inter-relationships are multifaceted: although obesity is a major risk factor for T2D, not all obese individuals will develop T2D. In a 2019 study, Thingholm et al. used 16S rRNA amplicon sequencing, shotgun metagenomic sequencing, and metabolomics to tease out how gut microbiota composition differed between non-obese non-diabetic, obese non-diabetic, and obese T2D individuals. They not only found that obesity is associated with increases and decreases in certain taxa but also identified a combined effect of dietary supplements and common medications on gut microbiota composition (3、4).
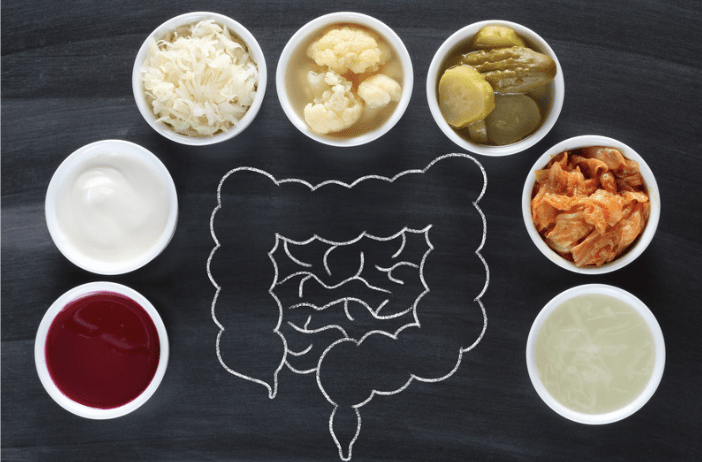
It’s high time we start focusing on real approaches to improve diet, nutrition, and human health. What range of microbial community compositions truly constitutes a healthy gut microbiota? Could beneficial microbes be added to foods to enhance a recipient’s gut microbiota? Would that approach be successfully implemented to enhance the body’s digestion, absorption, and metabolite production capabilities? (5, 6) A 2019 study by Redondo-Useros et al. used 16S rRNA amplicon sequencing to determine whether bacteria ingested from “probiotic” foods (probiotic fermented milk [PFM] and yogurts) are promoting long-lasting, “healthy” microbiota composition in the human gut. These results indicated that eating PFM and yogurt was associated with higher levels of ingested bacteria in the gut, particularly Bifidobacterium. This suggests that increased Bifidobacterium levels were beneficial for PFM consumption. (5)
The important question is whether certain health conditions associated with gut microbiota composition could be treated with probiotics. A 2022 study by Tian et al. related major depressive disorder (MDD) with dysfunctional gut motility. During a four-week random double-blinded controlled trial, MDD patients were administered a combined formula with three bacterial strains. This study has shown anti-depressive effects in mice. The treated participants showed a significant decrease in psychiatric and gastrointestinal symptoms than the control group (6) Although additional investigation and longer trials are needed but these findings suggest the possibility to boost and maintain “healthy” gut bacteria to treat diseases like obesity and diabetes.
The human body is a perfect habitat for the intestinal flora to flourish, which then helps the body to maintain normal physiological functions. Further analysis of the structure of intestinal flora and exploration of the roles of different microorganisms is direly needed to understand their functionalities and how they can be better utilized for the betterment of mankind. How to make full use of their different properties to improve human health should continue to be a focus of our attention in the future.
References
1. Tito, R. Y. et al. (2019) Population‑level analysis of Blastocystis subtype prevalence and variation in the human gut microbiota. Gut 68:1180.
2. Xie F. et al. (2021) Metagenomic sequencing reveals that high-grain feeding alters the composition and metabolism of cecal microbiota and induces cecal mucosal injury in sheep. mSystems 6(5):e00915.
3. Thingholm L. B. et al. (2019) Obese individuals with and without type 2 diabetes show different gut microbial functional capacity and composition. Cell Host & Microbe 26:252.
4. Bi Y. et al. (2021) Multiomics analysis reveals the presence of a microbiome in the gut of fetal lambs. Gut 70:853.
5. Redondo-Useros N. et al. (2019) Associations of probiotic fermented milk (PFM) and yogurt consumption with Bifidobacteria and Lactobacillus components of the gut microbiota in healthy adults. Nutrients 11:651.
6. Tian P. et al. (2022) Multi-probiotics ameliorate major depressive disorder and accompanying gastrointestinal syndromes via serotonergic system regulation. J. Adv. Res. doi.org/10.1016/j.jare.2022.05.003
7. Mitsuoka T. (1984) The effect of nutrition on intestinal flora. Nahrung 28(6-7):619.
